Are Tick Bites a Cause for Concern? Understanding Lyme Disease
Every summer, we all look forward to the time we’re going to spend outside with family and friends. Everything that puts a smile on our faces when we think of summer happens outside- beaches, hikes, playing with pets. With all the summer fun, though, we always seem to forget about all the pests that come out in summertime and all the insect bites we end up with… like tick bites.
Ticks are small parasites often found in wooded areas, grasslands, and areas with dense vegetation. Ticks bite humans and animals and can spread diseases, such as Lyme disease, through their bite. It is important to understand how to prevent tick bites and how to recognize signs of Lyme disease in the event of a bite so that you can seek treatment quickly.
What is Lyme Disease?

Lyme disease is an illness caused by borrelia bacteria. This bacterium transmits through the bite of a tick carrying the bacteria. This bacterium is common in parts of the United States, Europe, and Canada. Anyone who experiences a tick bite is at risk of developing symptoms of Lyme disease, which can prove serious, permanent, and even fatal if left untreated.
Symptoms
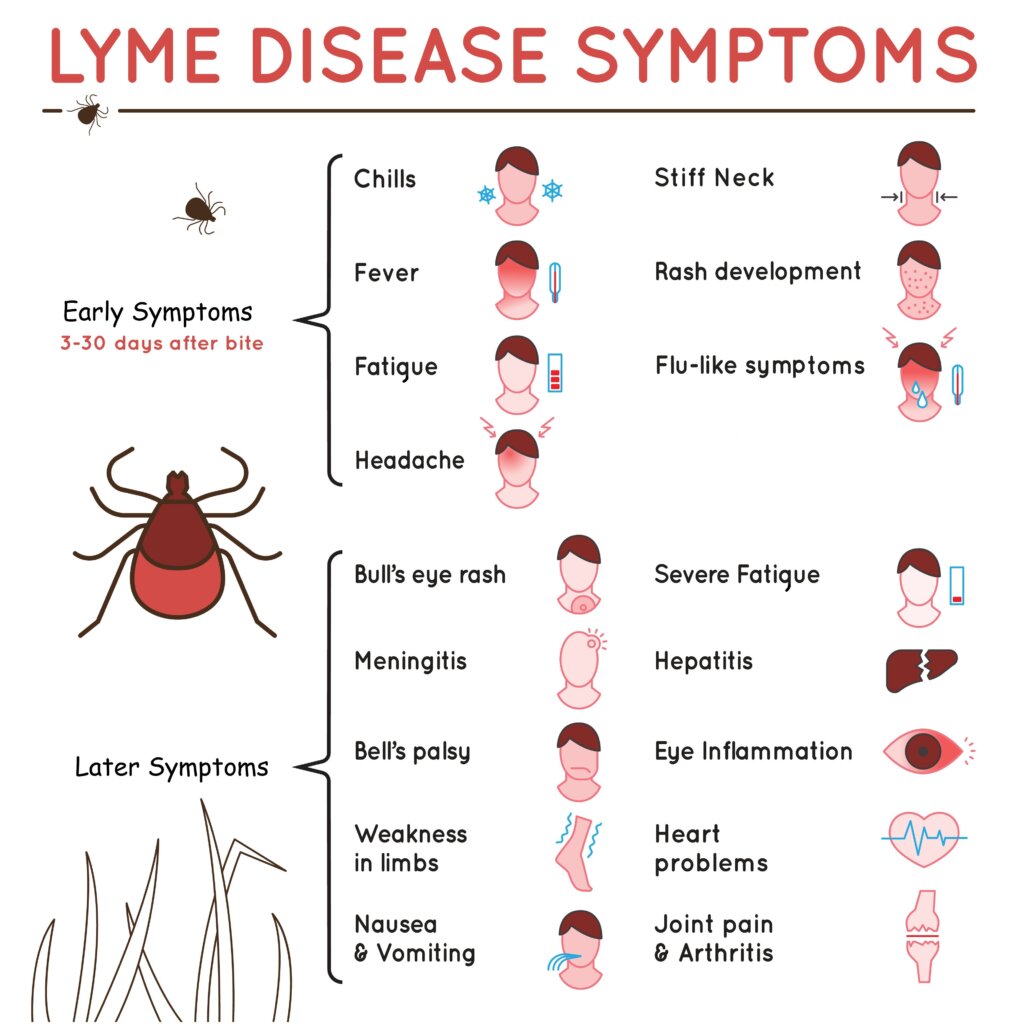
Symptoms of Lyme disease can vary and may develop in stages. Not everyone infected with Lyme disease will experience the same symptoms and some individuals may not display any symptoms at all. Common signs and symptoms associated with Lyme disease include:
Early Localized Stage:
- Erythema migrans (EM) rash: A circular or bull’s-eye-shaped rash that expands from the site of the tick bite. It may appear within 3 to 30 days after the bite and is typically not itchy or painful.
- Flu-like symptoms: Fever, fatigue, headache, muscle and joint aches, swollen lymph nodes, and general malaise.
Early Disseminated Stage:
- Multiple EM rashes: Additional rashes may develop in different areas of the body.
- Flu-like symptoms: Persistent fever, fatigue, headache, muscle and joint aches, and swollen lymph nodes.
- Neurological symptoms: Numbness or tingling in the extremities, facial paralysis (Bell’s palsy), meningitis (headache, stiff neck, sensitivity to light), and dizziness.
Late Disseminated Stage:
- Arthritis: Recurrent episodes of joint swelling, particularly in large joints like the knees.
- Neurological symptoms: Memory problems, difficulty concentrating, sleep disturbances, nerve pain, and neuropathy.
- Heart problems: Irregular heart rhythm, palpitations, and chest pain.
It’s important to note that these symptoms can overlap with other conditions, making a diagnosis challenging. If you experience any of these symptoms after a tick bite, seek medical attention for proper evaluation and diagnosis.
Without Treatment
If Lyme disease is left untreated, it can lead to more severe and potentially long-term complications. These complications can worsen as time goes on and can even become permanent if not addressed or addressed adequately. Severe complications may include chronic joint inflammation and arthritis, mobility issues, neurological complications, meningitis, heart abnormalities, serious cardiac issues, eye inflammation, hearing problems, memory impairment, mood changes such as depression and anxiety, and in rare cases- encephalitis and peripheral neuropathy.
How to Prevent Tick Bites & Lyme Disease
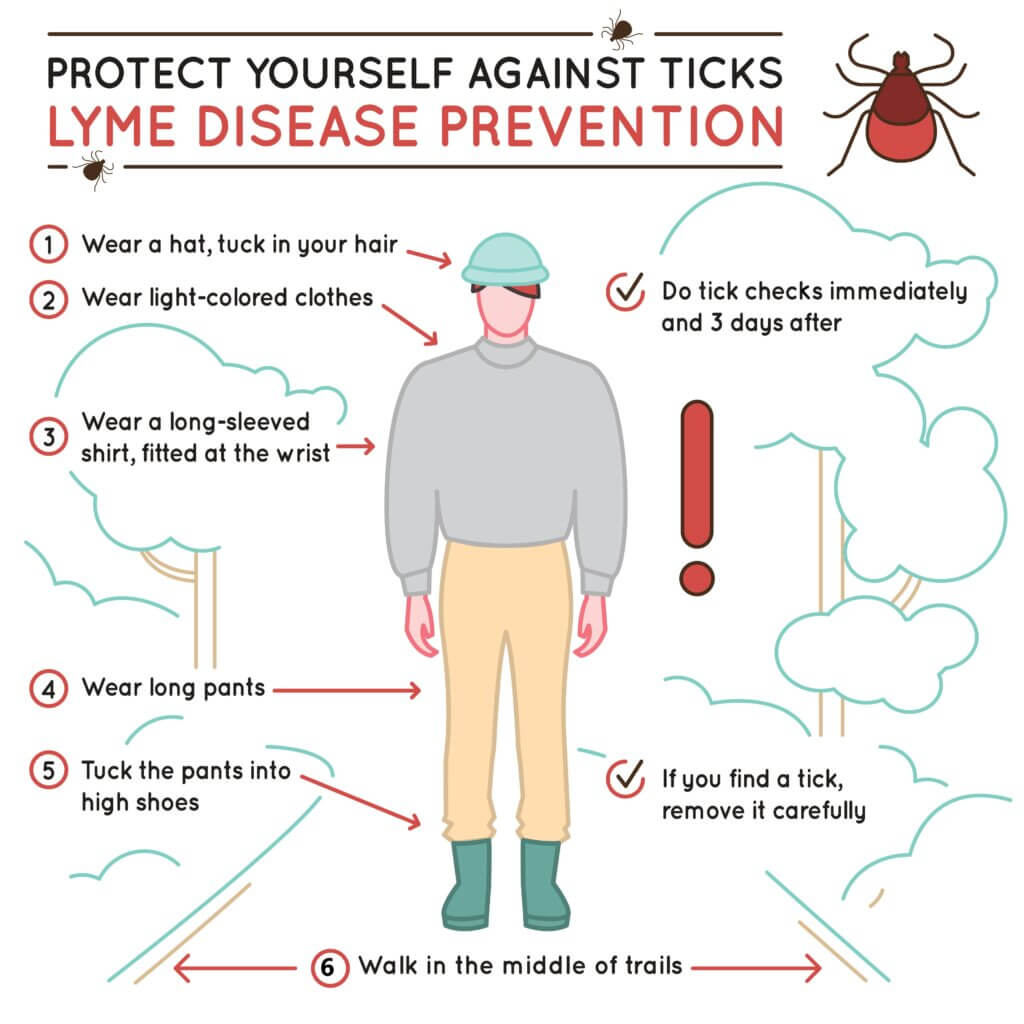
Lyme Disease can quickly become serious for those infected. It is important to be aware of simple ways to prevent tick bites and Lyme disease, such as:
- Avoid tick-infested areas: When possible, try to stay away from areas with high grass, dense vegetation, and leaf litter where ticks are commonly found. If you need to be in such areas, walk in the center of trails and avoid brushing against vegetation.
- Wear protective clothing: When spending time outdoors in tick-prone areas, wear long-sleeved shirts, long pants tucked into socks or boots, and a hat. Light-colored clothing can help you spot ticks more easily.
- Perform tick checks: After spending time in areas where ticks may be present, thoroughly check your body for ticks. Pay close attention to areas such as the scalp, behind the ears, armpits, groin, and behind the knees. Promptly remove any ticks you find.
- Shower after outdoor activities: Taking a shower within two hours of being outdoors can help wash away ticks that may be crawling on your body. Use a washcloth or loofah to help remove ticks that haven’t attached yet.
- Maintain a tick-free yard: Create a tick-safe environment by keeping your lawn well-maintained, removing leaf litter, and clearing tall grass and brush.
Our Approach
The Oxford Center has developed a Lyme Disease Treatment Program to help you on your way to recovery. Our program includes the following services:
Hyperbaric Oxygen Therapy (HBOT)

Traditional treatment for Lyme disease involves antibiotics in the form of either oral, injections, or IV. Co-infections frequently require a different treatment plan than antibiotic therapy as they are not always effective for Lyme disease. The bacteria associated with Lyme disease is very sensitive to oxygen and is debilitated in a highly oxygenated environment. Research shows that HBOT makes a significant improvement when used to treat Lyme disease, even with patients who have not been successful with antibiotic therapy. HBOT decreases inflammation, oxygenates the entire body, stimulates the growth of new healthy blood vessels, and releases stem cells up to 800% more after twenty sessions. Research shows that the efficiency of antibiotics in the case of Lyme Disease has increased as new blood vessel growth allows the medication to penetrate deeper into tissues.
Neurofeedback Therapy

A Quantitative EEG shows us the electrical activity of the brain. We will be able to see if inflammation is present, if there are any areas of hyper- or hypoactivity, and any areas of disconnect. Patients with Lyme disease may experience Post Treatment Lyme Disease Syndrome (PTLDS) and may experience pain, neurocognitive or fatigue symptoms, headaches, brain fog, and sleep disorders. PTLDS seems to occur more frequently after Lyme disease has caused neurological complications. Research suggests that the brain becomes more sensitive to pain signals and does not reset after the infection, causing the increased sensitivity to continue. Using the information from the QEEG, we can focus on the area(s) of the brain most affected and bring those areas back into balance through Neurofeedback Therapy.
Nutrition Services

Finally, nutrition helps to address co-infections associated with Lyme disease. Our services will look to heal the gut, look at what is wrong, and support your body in anything else going on. Gut healing is a great tool in your health journey, and it can be essential to addressing every issue going on in your body. Nutrition coaching provides the information and support you need to learn to enjoy health-building foods, create a healthy living environment, and feel good in your body.